Neurointerventional Services
Interventional Neuroradiology (also known as Neurointerventional Surgery or Endovascular Neurosurgery) is a sub-specialty that performs minimally invasive procedures to diagnose and treat diseases of the brain, head, neck, and spine. Neurointerventional procedures use state-of-the-art devices and image-guided techniques to deliver treatments through a small puncture in the skin of the groin or arm instead of open surgery.
Additional information is available by clicking on the links below.
Brain Aneurysms
- Ruptured (Subarachnoid Hemorrhage) and Unruptured Aneurysm Embolizations
- Aneurysm Coiling
- Balloon Assisted Aneurysm Coiling
- Stent Assisted Aneurysm Coiling
- Pipeline Embolization Device Placement for Treatment of Unruptured Aneurysms
Artery Stenosis
Venous Stenosis
Vascular Malformations
- AVM and AVF Embolization with Liquid Embolisates, including Onyx and n-BCA
- Brain Arteriovenous Malformation (AVM) Embolization
- Dural Arteriovenous Fistula (AVF) Embolization
- Spinal AVF Embolization
Brain Tumors
Ischemic Stroke
- Stent Retriever with Flow Restoration
- Clot Extraction using Aspiration Systems (ADAPT technique)
- Intra-arterial Thrombolysis (IA t-PA& IA abciximab/Reopro)
- Intracranial Angioplasty and Stenting
- Cerebral Venous Thrombosis (CVT) Thrombolysis & Thrombectomy
Brain Aneurysms
Ruptured (Subarachnoid Hemorrhage) and Unruptured Aneurysm Embolizations
An intracranial aneurysm (also called cerebral or brain aneurysm) is a cerebrovascular disorder in which weakness in the wall of a cerebralartery or vein causes a localized dilation or ballooning of the blood vessel.
If an aneurysm ruptures, blood leaks into the thin coverings of the brain called the subarachnoid space. This is called a subarachnoid hemorrhage. This classically presents as a sudden, severe headache (ie. “thunderclap headache”) worse than any previous headaches.
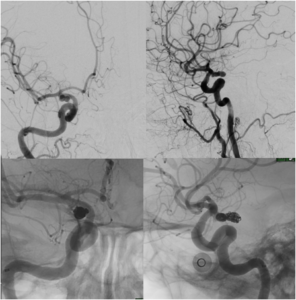
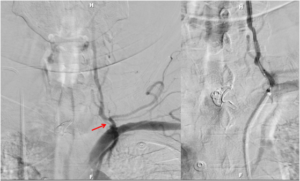
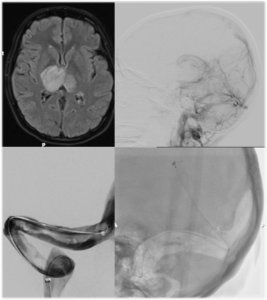
Aneurysm Coiling
Aneurysm coiling refers to the insertion of platinum coils into the aneurysm. A catheter is inserted into a blood vessel and passed using X-ray guidance through the circulation into the brain and then into the aneurysm sac. The microcoils are pushed into the aneurysm through the catheter. Upon depositing within the aneurysm, the coils initiate a thrombotic reaction within the aneurysm. If successful, this prevents further bleeding from the aneurysm.
Balloon Assisted Aneurysm Coiling
Balloon assisted aneurysm coiling is a technique in which a small balloon is inflated within the parent artery of the aneurysm to provide a scaffolding for the coils. This allows for the safe and effective treatment of aneurysm with a broad base (or neck) and with more complex anatomy. a stent may be passed first into the parent artery to serve as a scaffold for the coils.
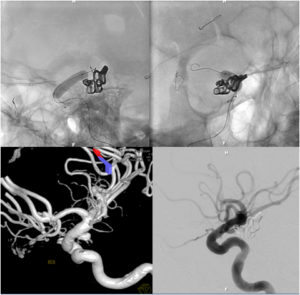
 Stent Assisted Aneurysm Coiling
Stent Assisted Aneurysm Coiling
Stent assisted aneurysm coiling is a technique in which a stent, or tubular piece of mesh, is deposited within the parent artery of the aneurysm to provide a scaffolding for the coils. This allows for the safe and effective treatment of aneurysm with a broad base (or neck) and with more complex anatomy. Placement of an intracranial stent will require administration of anti-platelet drugs, such as aspirin, clopidogrel, or prasugrel.
Pipeline Embolization Device Placement for Treatment of Unruptured Aneurysms
Flow diversion is an endovascular technique, used primarily for the treatment of unruptured intracranial aneurysms, whereby a tubular piece of mesh with very small interstices or “flow diverter” is placed inside the parent blood vessel to divert blood flow away from the aneurysm itself.
During a flow-diversion procedure procedure, a microcatheter is navigated beyond the aneurysm without having to enter the aneurysm sac itself. The flow-diverting device is then carefully deployed across the neck of the aneurysm in the parent blood vessel. The only currently approved FDA flow diverting device is the Pipeline™ Embolization Device (PED).
Artery Stenosis
 Carotid Artery Angioplasty & Stenting
Carotid Artery Angioplasty & Stenting
Carotid artery angioplasty and stenting is performed for the treatment of carotid artery stenosis. The technique of the procedure involves mechanically widening narrowed or obstructed carotid arteries that is usually the result of atherosclerosis. An empty and collapsed balloon on a guide wire, known as a balloon catheter, is passed into the narrowed carotid artery and then inflated to a fixed size. The balloon forces expansion of the blood vessel wall for improved flow, and the balloon is then deflated and withdrawn. A stent (tubular piece of mesh) is then routinely deposited to ensure that the vessel remains open. An embolization protection device may be used during the procedure to prevent the atherosclerotic plaque from the narrowed vessel wall from migrating to the brain and causing symptoms of stroke.

Intracranial Angioplasty & Stenting
Intracranial angioplasty and stenting is performed for the treatment of stenosis of an intracranial artery that is causing recurrent strokes and/or TIA’s that are refractory to optimal medical management (ie. medical control of hypertension,diabetes, and dyslipidemia in conjunction with dual antiplatelet therapy).

The procedural is technically similar to that described for carotid artery angioplasty and stenting, although the angioplasty balloons and intracranial stents are smaller and more flexible than those used in the cervical circulation.
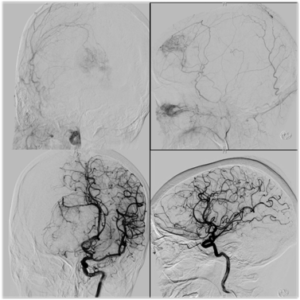
Venous Stenosis
Angioplasty and Stenting for Dural Venous Sinus Stenosis and Idiopathic Intracranial Hypertension / PseudotumorCerebri
 Idiopathic intracranial hypertension (IIH), sometimes called by the older names benign intracranial hypertension (BIH) or pseudotumorcerebri (PTC), is a neurological disorder that is characterized by increased intracranial pressure (pressure around the brain) in the absence of a tumor or other disease. The symptoms are headache, nausea, and vomiting, and sometimes pulsatiletinnitus (buzzing in the ears synchronous with the pulse), diplopia(double vision) and other visual symptoms. The increased pressure may lead to swelling of the optic disc in the eye. Swelling of the optic disc can progress to vision loss.
Idiopathic intracranial hypertension (IIH), sometimes called by the older names benign intracranial hypertension (BIH) or pseudotumorcerebri (PTC), is a neurological disorder that is characterized by increased intracranial pressure (pressure around the brain) in the absence of a tumor or other disease. The symptoms are headache, nausea, and vomiting, and sometimes pulsatiletinnitus (buzzing in the ears synchronous with the pulse), diplopia(double vision) and other visual symptoms. The increased pressure may lead to swelling of the optic disc in the eye. Swelling of the optic disc can progress to vision loss.
Older treatments of IIH included repeat lumbar punctures, medications that decrease production of CSF, surgical decompression of the optic nerve (optic nerve sheath fenestration), surgical shunting of the CSF from the spine to the abdomen (lumboperitoneal shunt), CSF shunting from the brain to the abdomen (ventriculoperitoneal shunt), and even CSF shunting from the brain to the heart (ventriculoatrial shunt).
New research demonstrates excellent clinical outcomes for the treatment of IIH by minimally invasive endovascular methods. These endovascular treatments involve placement of intracranial angioplasty balloons and stents across areas of narrowing (stenosis) within the cerebral venous circulation that remove blockages and relieve the elevated intracranial pressure.
Vascular Malformations
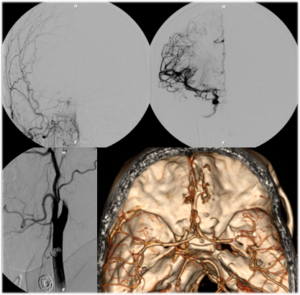
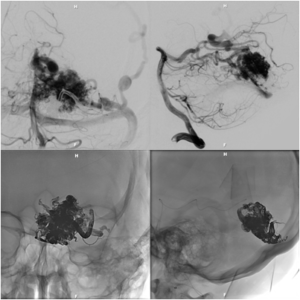 Brain Arteriovenous Malformation (AVM) Embolization
Brain Arteriovenous Malformation (AVM) Embolization
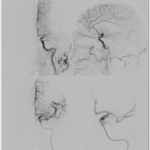
An Arteriovenous malformation or AVM is an abnormal connection between arteries and veins, bypassing the capillary system. This vascular anomaly is widely known because of its occurrence in the central nervous system, but can appear in any location. Although many AVMs are asymptomatic, AVMs in the brain can cause intense headache, intracranial bleeding, and/or lead to other serious medical problems, such as seizures. Vascular malformations can be treated endovascularly with embolization using liquid embolics, such as Onyx and n-BCA, by open surgery, or by gamma knife radiosurgery. Sometimes these lesions are treated by a combination of the above mentioned therapies.
 Dural Arteriovenous Fistula (AVF) Embolization
Dural Arteriovenous Fistula (AVF) Embolization
A duralarteriovenous fistula (DAVF) is an abnormal direct connection (fistula) between a meningealartery and a meningeal vein or dural venous sinus. Like other vascular malformations, a dural AVF can be treated endovascularlywith embolization using liquid embolics, such as Onyx and n-BCA, by open surgery, or by gamma knife radiosurgery. Sometimes these lesions are treated by a combination of the above mentioned therapies.
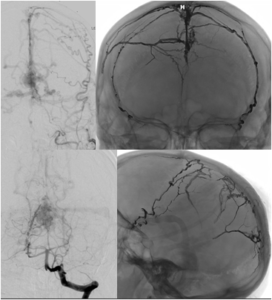
Spinal AVF Embolization
 Most spinal fistulas are created when a radiculomeningeal artery feeds directly into a radicular vein near the spinal nerve root. Spinal dural AVFs are most commonly found in the thoracolumbar region. Patients become symptomatic because the AVF creates spinal cord venous congestion and hypertension, resulting in hypoperfusion, hypoxia, and edema of the spinal cord. Due to the slow-flow nature of most spinal dural AVFs, hemorrhage rarely occurs. Most dural AVFs are believed to occur spontaneously, but the exact etiology is still unknown. Again, these types of vascular lesions can be treated endovascularly with embolization using liquid embolics, such as Onyx and n-BCA, and with open surgery.
Most spinal fistulas are created when a radiculomeningeal artery feeds directly into a radicular vein near the spinal nerve root. Spinal dural AVFs are most commonly found in the thoracolumbar region. Patients become symptomatic because the AVF creates spinal cord venous congestion and hypertension, resulting in hypoperfusion, hypoxia, and edema of the spinal cord. Due to the slow-flow nature of most spinal dural AVFs, hemorrhage rarely occurs. Most dural AVFs are believed to occur spontaneously, but the exact etiology is still unknown. Again, these types of vascular lesions can be treated endovascularly with embolization using liquid embolics, such as Onyx and n-BCA, and with open surgery.
Brain Tumors
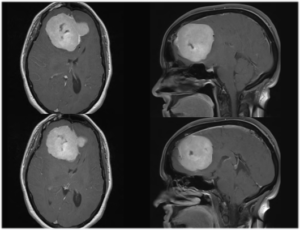
 Intracranial and Extracranial Tumor Embolizations
Intracranial and Extracranial Tumor Embolizations
Various tumors in the brain, head, neck, and spine can be treated pre-operatively with embolization to reduce the risk of bleeding during open surgery.
The list of tumors amenable to this therapy is very broad and includes meningiomas, glomus tumors, paragangliomas, nasopharyngeal angiofibromas, as well as metastatic cancerous tumors from the lung, breast, kidney, skin, and bowel. The procedure involves selection of the small arteries that supply blood flow to the tumor followed by the injection of small particles to reduce blood flow and induce ischemia within the tumor tissue.
 Intra-Arterial Chemotherapy
Intra-Arterial Chemotherapy
Intra-arterial infusion of chemotherapy is reserved for primary malignant tumors of the brain, head, neck, and spine. In particular, this treatment may provide benefit for patients with glioblastomamultiforme. As with other tumor embolizations,the procedure involves selection of the small arteries that supply blood flow to the tumor. An agent is then administered to break down the blood-brain barrier.
After administration of this agent, the chemotherapeutic agent is then administered and may penetrate the tumor cells.
Ischemic Stroke
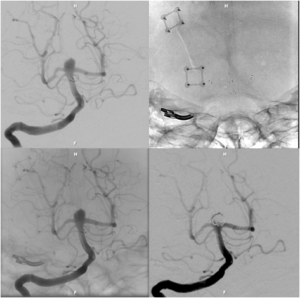
 Stent Retriever with Flow Restoration
Stent Retriever with Flow Restoration
A stent is a tubular piece of mesh that can be placed inside of a blood vessel to maintain the blood vessel’s patency. In the setting of acute ischemic stroke, stent placement enables entrapment of the thrombus between the stent and the vessel wall to provide fast recanalization and to restore antegrade blood flow.
Flow restoration may rapidly re-establish oxygen supply in the brain region that has been deprived of the oxygen and nutrients that the blood supplies and removes the metabolic biproducts that are produced. Flow restoration also enhances the efficacy of thrombolytic drugs (ie. clot busters).
“Stent retrievers”, as they have been named, are a technology that haverevolutionalized the treatment of acute ischemic stroke. Stent retrievers allow thrombectomy to be performed by first deploying the stent inside of the clot and then pulling back the deployed stent into the guide catheter. In this scenario, the struts of the stent engage the thrombotic material and allow removal of the clot for the patient’s body.
Particularly advantageous is that the stent is applicable repeatedly and can be used even in small peripheral vessel branches (eg, M2 segments). In contrast with conventional stent systems, stent retrievers require no anticoagulation, as the stent is not deployed permanently.
Clot Extraction using Aspiration Systems (ADAPT technique)
The ADAPT technique is a new method for the treatment of acute ischmemic stroke that utilizes direct aspiration on the first pass with an extremely flexible and trackable large bore aspiration catheter as the primary method for vessel recanalization. Initial results with this technique have resulted in favorable patient outcomes.
 Intra-arterial Thrombolysis (IA t-PA& IA abciximab/Reopro)
Intra-arterial Thrombolysis (IA t-PA& IA abciximab/Reopro)
One of the main limitations to IV tPA (ie. “clot busting” medicine injected into a vein in the arm) has been the strict 3-hour time window for initiating therapy. This short time window, combined with a lack of public awareness of stroke, has unfortunately limited the use of IV thrombolysis. Intraarterial thrombolysis (IAT) (ie. “clot busting” medicine injected into the artery right at the face of the clot) has been studies as an alternative to IVT.
The idea behind IAT is rapid local delivery of thrombolytic agent through a microcatheter placed near the site of occlusion. This should lead to improved recanalization and reduced hemorrhagic complications. The major disadvantages to IAT include the complexity of the procedure, the level of required technical expertise, relatively selective availability, delays in initiating treatment, and the additional risks and expense of an invasive procedure compared with IVT.

Intracranial Angioplasty & Stenting
Intracranial angioplasty and stenting is performed for the treatment of stenosis of an intracranial artery that is causing recurrent strokes and/or TIA’s that are refractory to optimal medical management (ie. medical control of hypertension,diabetes, and dyslipidemia in conjunction with dual antiplatelet therapy).

The procedural is technically similar to that described for carotid artery angioplasty and stenting, although the angioplasty balloons and intracranial stents are smaller and more flexible than those used in the cervical circulation.
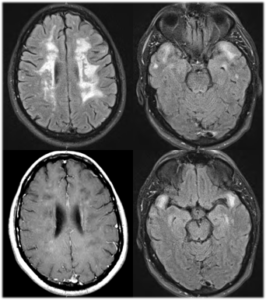
 Cerebral Venous Thrombosis (CVT) Thrombolysis & Thrombectomy
Cerebral Venous Thrombosis (CVT) Thrombolysis & Thrombectomy
Cerebral venous sinus thrombosis is the presence of a blood clot in the dural venous sinuses, which drain blood from the brain. Symptoms may include headache, abnormal vision, any symptoms of stroke, and seizures. Treatment is medically with anticoagulants and rarely by endovascular methods, including thrombectomy and/or thrombolysis (enzymatic destruction of the blood clot).Thrombectomy and thrombolysis are only used in patients who deteriorate despite optimal medical treatment when other causes of deterioration have been eliminated. Bleeding into the brain is a major concern in the use of thrombectomy/thrombolysis.